Abstract
Background: Over the past decades, non-Hodgkin lymphoma (NHL) patients have significant improvement in the 5-year relative survival rate. In elderly NHL patients, comorbidities play a major role in mortality. Studies have shown that lower survival rates are multifactorial and strongly associated with certain races, gender, socioeconomic status, and availability of rituximab. Therefore, we aim to assess the differences in causes of mortality among races and genders. To better understand environmental contributions to one-year survival rate in NHL patients state-wise in the US, we examined the mortality-to-incidence rate (MIR) in senior NHL patients characterized by race, gender, and American health ranking (AHR) index.
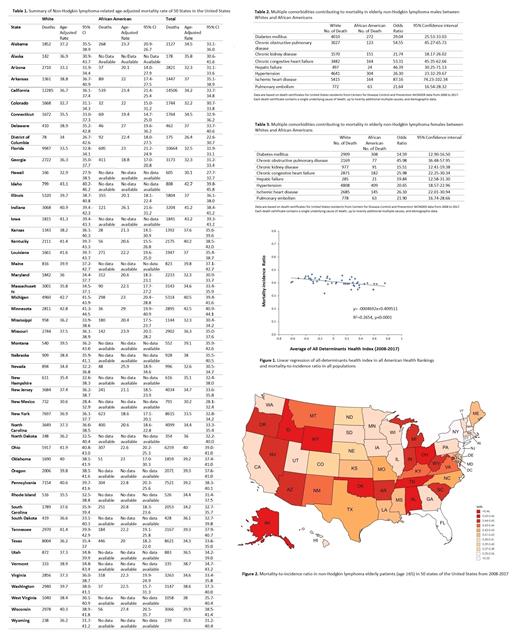
Methods: This is a retrospective study using the Centers for Disease Control and Prevention database from 2008 to 2017. Patients ≥65 years with non-Hodgkin lymphoma were included. AHR assesses the nation's health on a state-by-state basis to determine state health rankings with a composite index of health measures. AHR consists of five weighted core measures (four groups of health determinants and one health outcome): (1). Behaviors including excessive drinking, obesity, smoking, (2). Community and environment including air pollution, poverty, infectious disease, violent crime, (3). Policy including immunization, public health funding, uninsured rate, (4). Clinical care including primary care physicians, mental health providers, preventable hospitalizations, and (5). Outcomes including cancer deaths, cardiovascular deaths, diabetes, disparity in mental status. A ten-year (2008-2017) average of all-determinants value from AHR were reported and MIR, a parameter that can serve as a proxy for survival, was compared between US states. We analyzed the association between NHL mortality and state health disparities using linear regression. Multiple-cause-of-death data is based on death certificates for US residents. Each death certificate contains a single underlying cause of death, up to twenty additional multiple causes, and demographic data. We analyzed the multiple cause age-adjusted mortality rate in White males and females versus African American males and females. All data were analyzed using R version 4.0.5, with p-values <0.05 in two-sided t-tests to indicate statistical significance.
Results: In this 10-year analysis, the mean age-adjusted mortality rate (AAMR) in Whites, African Americans, and all populations were 38.2, 21.4, and 36.7 per 1,000,000 population, respectively. Among all 50 states, Idaho had the highest AAMR for all populations (42.7/1,000,000) and Whites (43.1/1,000,000); Minnesota had the highest AAMR for African Americans (29/1,000,000). District of Columbia had the lowest AAMR for all populations (26.4/1,000,000); New Mexico had the lowest AAMR for Whites (30.6/1,000,000) and New York had the lowest AAMR for African Americans (Table 1). Our results demonstrated that elderly NHL patients in states with better health all-determinants index had significantly lower MIR in all populations (R 2=0.2654, p <0.001, Figure 1). The three lowest MIR states in the US were Florida (0.319), Connecticut (0.348), and New York (0.348) (Figure 2). Whites were more likely to have underlying comorbidities than African Americans, especially ischemic heart disease (Male: OR 87.16, 95% CI 74.23-102.34; Female: 26.10, 95% CI 22.01-30.94), congestive heart failure (Male: OR 53.31, 95% CI 45.35-62.66; Female: OR 25.98, 95% CI 22.25-30.34), and chronic obstructive pulmonary disease (Male: OR 54.55, 95% CI 45.27-65.73; Female: OR 45.98, 95% CI 36.48-57.95) (Table 2,3).
Conclusions: States of better health index in terms of all determinants had lower MIR for elderly NHL patients in the US. Factors contributing to the difference in MIR possibly include variations in socioeconomic status, insurance coverage, and healthcare access. Our results highlight the need to focus on secondary prevention to decrease morbidities and health disparities in NHL patients.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal